Atherosclerosis of the carotid arteries
Table of content

Epidemiology of carotid atherosclerosis
Carotid atherosclerosis is a disease that is one of the main causes of strokes worldwide. The prevalence of carotid atherosclerosis varies significantly depending on geographic location, lifestyle, and ethnicity of the population.
Geographical differences
North America and Europe demonstrate a high prevalence of carotid atherosclerosis. Research shows that up to 10% of the elderly population in these regions suffers from this disease. This may be due to high rates of comorbidities such as hypertension and diabetes, as well as a high standard of living that is often accompanied by less physical activity and an unhealthy diet.
Asian countries are also experiencing an increase in the incidence of carotid atherosclerosis, which correlates with urbanization and changes in lifestyle. In Japan and China, for example, rapid industrial development and changes in diet to a more Western style have led to an increase in the incidence of atherosclerosis.
Low- and middle-income countries often show a lower prevalence of carotid atherosclerosis, which may be due to the younger age of the population and higher physical activity. However, these regions have seen an increasing trend in cases with urbanization and deteriorating nutrition.
Factors influencing prevalence
The degree of urbanization and changes in the lifestyle of the population.
Availability and quality of medical care, which affect the possibility of early detection and treatment of diseases that provoke atherosclerosis.
National programs to combat smoking, level of education and economic development, which directly affect the health of the population.
Thus, carotid atherosclerosis is a multifactorial disease influenced by multiple socioeconomic and cultural factors that need to be taken into account when developing prevention and treatment measures at the national and international levels.
Etiology of atherosclerosis
The main risk factors for the development of atherosclerosis are hypertension, diabetes, smoking, hyperlipidemia and family history. Each of these factors contributes to damage to the vascular endothelium, which initiates the formation of atherosclerotic plaques. Age and gender also play a significant role; the risk increases with age; men are more susceptible to this disease.
Pathophysiology of atherosclerosis
Atherosclerosis is a chronic disease of the arteries, characterized by impaired lipid and protein metabolism, inflammation and the subsequent formation of atherosclerotic plaques, which can lead to stenosis and vascular occlusion. The development of atherosclerosis can be divided into several key stages:
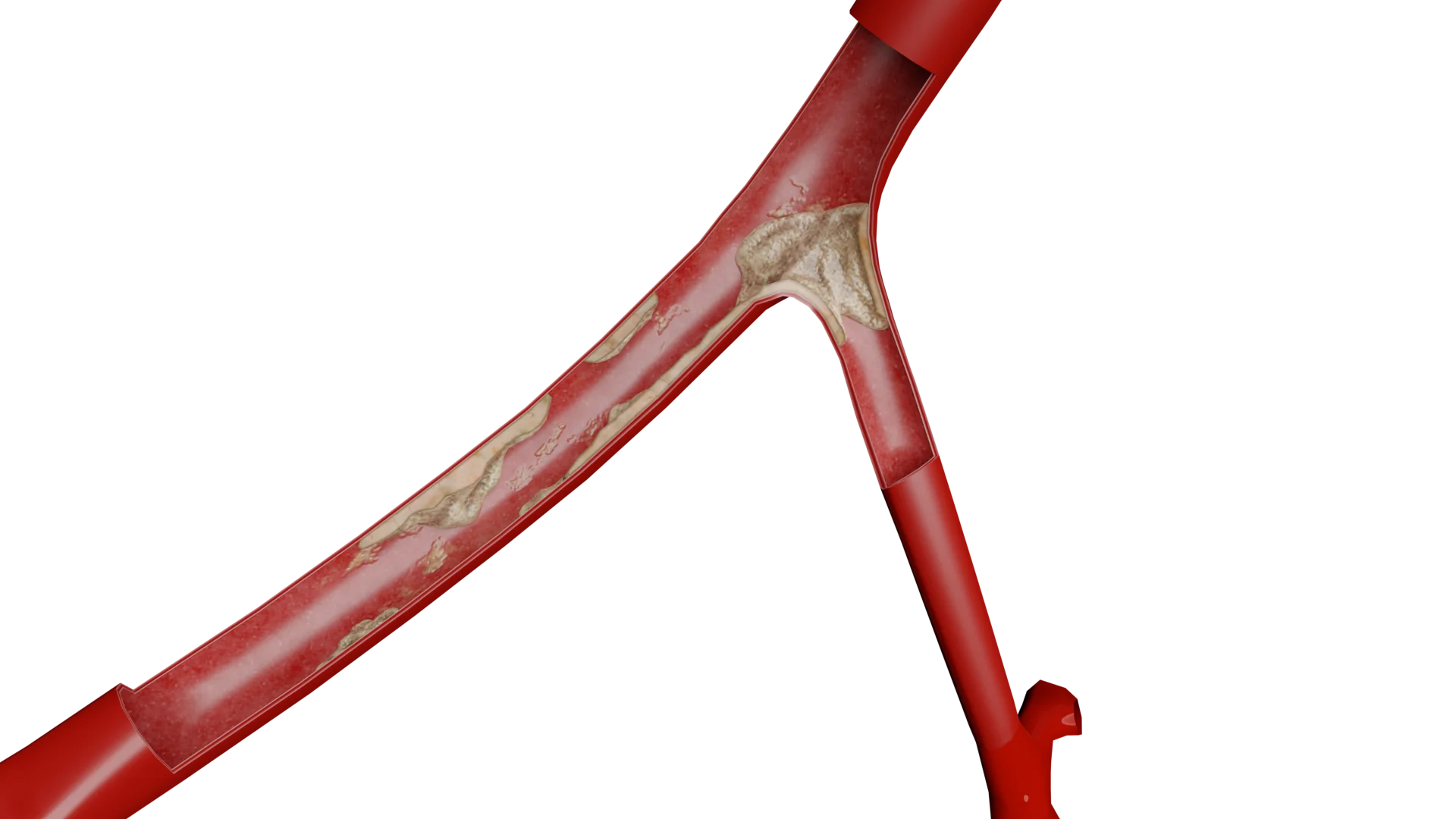
Endothelial dysfunction: The primary event in the development of atherosclerosis is damage to the endothelium, the inner layer of the arterial wall. Endothelial dysfunction can be caused by a variety of factors, including hypertension, smoking, hyperglycemia, and oxidative stress. Damaged endothelium loses its barrier function, which increases permeability to low-density lipoproteins (LDL).
LDL oxidation: Under the influence of oxidative processes, LDL is converted into oxidized LDL (ox-LDL), which has direct cytotoxicity and contributes to the progression of atherogenesis. These modified lipoproteins activate the endothelium and attract monocytes.
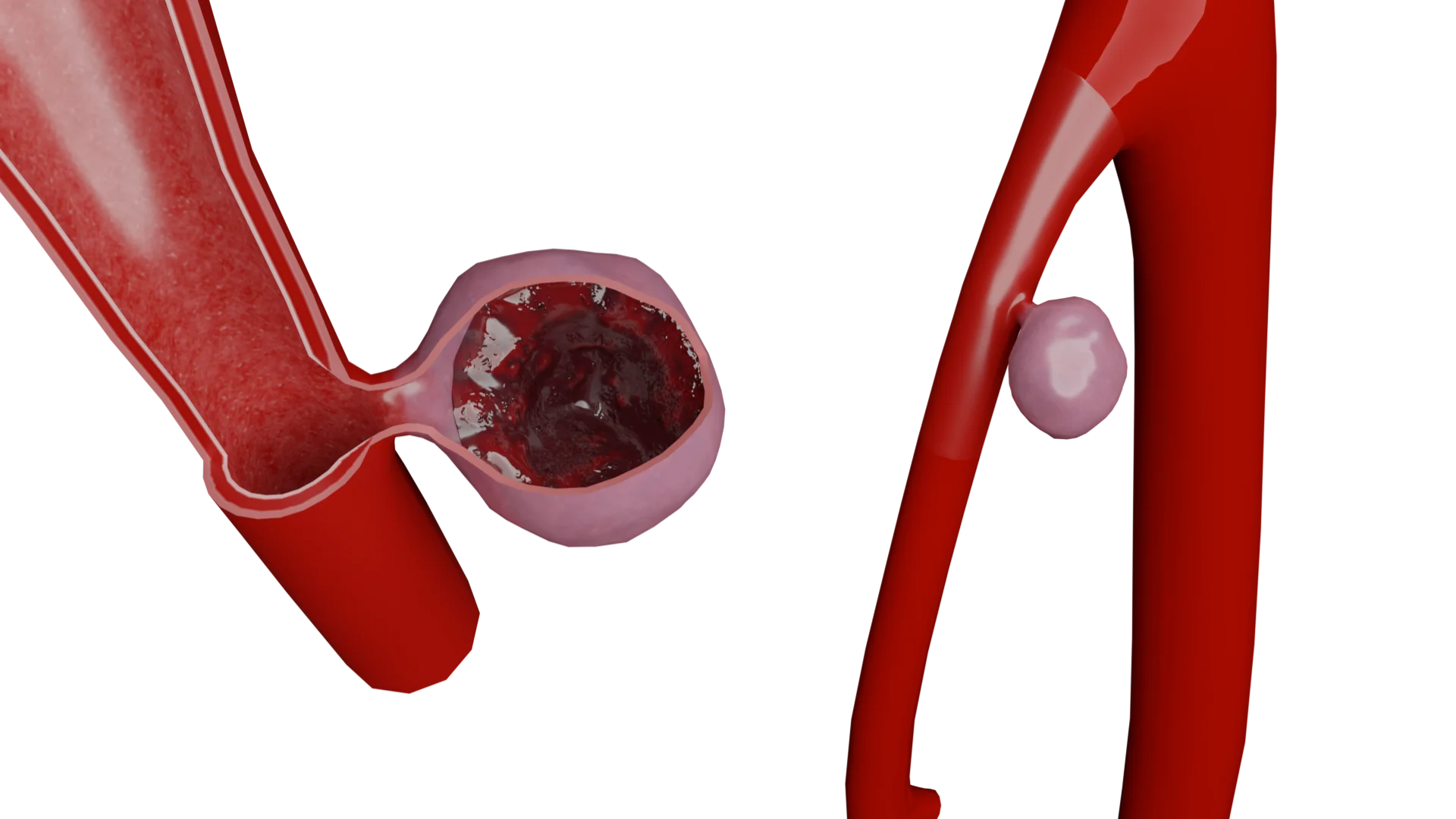
Inflammation and foam cell formation:Monocytes that penetrate the arterial wall differentiate into macrophages, which take up oxidized LDL and turn into foam cells. The accumulation of foam cells leads to the formation of a fatty spot, which is an early morphological manifestation of atherosclerosis.
Proliferation of smooth muscle cells and formation of fibrous capsule: In response to inflammation and damage to the vascular wall, smooth muscle cells migrate from the tunica media to the intima, where they proliferate and produce collagen and other extracellular matrix components. This leads to thickening of the intima and the formation of a fibrous capsule of an atherosclerotic plaque.
Complications of atherosclerotic plaque:Over time, atherosclerotic plaque can become unstable and rupture, leading to thrombus formation and acute vascular occlusion. This can cause acute clinical manifestations such as acute cerebrovascular accident.
Clinical manifestations
In the early stages, atherosclerosis of the carotid arteries can be asymptomatic. As the disease progresses and significant stenosis develops, transient ischemic attacks or ischemic stroke occur. Symptoms include sudden numbness or weakness of the face, arm or leg, especially on one side of the body, difficulty speaking, seeing or coordinating.
Diagnostics
Diagnosis of atherosclerosis of the carotid arteries includes a number of instrumental and laboratory methods that help not only to detect the presence of plaques, but also to assess the degree of vascular damage and the risk of complications.
Instrumental diagnostic methods
Ultrasound examination with Dopplerography:
Indications: Suspicion of atherosclerosis of the carotid arteries, the presence of symptoms of transient ischemic attack or stroke, as well as the presence of risk factors (hypertension, diabetes, hyperlipidemia).
Signs: Presence of atherosclerotic plaques, narrowing of the artery lumen, change in blood flow speed in the area of stenosis.
Magnetic resonance angiography:
Indications: The need for high-precision arterial imaging to assess the degree of stenosis and vascular anatomy, especially in complex or equivocal cases.
Signs: Images can show the exact structure of the plaque and the extent and distribution of stenosis.
Computed tomography (CT angiography):
Indications: Suspicion of the presence of calcified plaques, the need to evaluate the possibility of surgical intervention.
Signs: CT is capable of assessing calcifications within plaques and accurately assessing the degree of stenosis.
Laboratory diagnostic methods
Lipid profile:
Indicators: Total cholesterol, HDL, LDL and triglycerides.
High levels of LDL and low levels of HDL increase the risk of developing atherosclerosis. High triglycerides are also associated with an increased risk.
Inflammatory markers (C-reactive protein):
Assess the degree of systemic inflammation that may contribute to the progression of atherosclerosis. Elevated CRP is associated with an increased risk of cardiovascular events.
Homocysteine:
Study of homocysteine levels in the blood, especially if there is a family history of early atherosclerosis or thrombosis. High homocysteine levels may contribute to endothelial dysfunction and increase the risk of atherosclerosis.
These diagnostic methods allow not only to accurately determine the presence of atherosclerosis of the carotid arteries, but also to assess the risk of developing serious complications such as stroke, which is key to determining treatment tactics and preventing the disease.
Treatment of atherosclerosis of the carotid arteries
Understanding the mechanisms of atherosclerosis is key to developing targeted therapeutic strategies. It is important to note that although some factors, such as genetic predisposition, cannot be changed, many aspects of the etiology of atherosclerosis can be controlled through lifestyle changes and drug interventions.
Treatment begins with lifestyle modification and drug therapy, including statins, antiplatelet agents and antihypertensive drugs. In case of significant stenosis or symptomatic disease, interventional methods are used, such as carotid angioplasty and stenting. In more severe cases, carotid endarterectomy may be required.
Carotid angioplasty and stenting
Step-by-step process of carotid artery stenting
How it's done: The procedure involves inserting a catheter through the femoral or radial artery to the site of carotid artery stenosis. A balloon is then inserted through the catheter, which is inflated to widen the narrowed section of the artery, after which a stent is installed in this place to maintain the lumen of the artery.
Indications: Symptomatic carotid artery stenosis ≥ 50% if surgical risks are increased or there are anatomical complications. Asymptomatic stenosis ≥ 60-70%, with a high risk of surgical complications or limited access to the artery.
Contraindications: Severe calcification of the artery wall, acute infectious diseases, poor blood clotting.
Results: The effectiveness is comparable to surgery in reducing the risk of stroke, but there is a risk of restenosis in the long term.
Direct endovascular hybrid surgery
How it is performed: Combination of open surgery and stenting. First, the surgeon directly accesses the carotid artery, and then the endovascular surgeon performs stenting.
Indications: Severe stenosis or occlusion of the carotid arteries, especially if accompanied by stenosis of other large vessels of the head and neck. Patients in whom traditional stenting or surgery is not appropriate due to high risk or anatomical conditions.
Contraindications: Similar contraindications for standard stenting.
Results: Allows you to more accurately control the process of restoration of the vascular lumen and reduces the risk of complications.
Standard carotid endarterectomy
How it is done: The surgeon makes an incision in the neck in the area of the affected carotid artery, opens the artery and removes the atherosclerotic plaque along with the inner lining of the artery. After the plaque is removed, the artery is sutured.
Indications: Symptomatic stenosis ≥ 50% by NASCET criteria or ≥ 70% by ECST criteria. Asymptomatic stenosis ≥ 60% with a life expectancy of more than 5 years and low surgical risk.
Contraindications: Absence of pronounced symptoms with minor stenosis, severe concomitant diseases.
Results: Reduce the risk of stroke by 50% or more compared to drug treatment.
Eversion carotid endarterectomy
How it is performed: It can be the method of choice when standard carotid endarterectomy is difficult due to anatomical features or when it is necessary to minimize tissue trauma. In the eversion technique, the surgeon "turns out" the inner lining of the artery, starting from the branching site. This allows the atherosclerotic plaque to be removed together with the inner lining of the artery entirely, minimizing trauma and the need for additional vessel prosthetics.
Indications and contraindications: Similar to standard carotid endarterectomy, but preferred when the risk of traditional surgery is high due to anatomical or physiological features.
Results: Allows to achieve results similar to classical surgery, while reducing the risk of surgical complications and accelerating the patient’s recovery.
General contraindications
Absolute contraindications: Current or recent stroke with massive neurological deficit. Unstable medical conditions such as acute heart failure or uncontrolled hypertension.
Relative contraindications: Serious concomitant diseases that significantly reduce life expectancy. Diffuse vascular diseases that complicate surgical access or increase the risk of procedural complications.
For a more detailed study of the indications and contraindications for this disease in order to reduce the risk of ischemic events and optimize clinical outcomes for patients with carotid atherosclerosis, we recommend referring to the recommendations of internationally recognized medical organizations. For example, these include: American Heart Association and European Society for Vascular Surgery.
External sources
VOKA catalogue.
https://catalog.voka.io/
Thapar, A., Jenkins, I. H., Mehta, A., & Davies, A. H. (2013). Diagnosis and management of carotid atherosclerosis.
BMJ, 346, f1485. Doi: 10.1136/bmj.f1485
Goethem, J. V., Hatsukami, T., Rothwell, P., Brown, M. M., & Moody, A. R. (2021). Roadmap consensus on carotid artery plaque imaging and impact on therapy strategies and guidelines: An international, multispecialty, expert review and position statement.
American Journal of Neuroradiology, 42(9): 1566–1575. Doi: 10.3174/ajnr.A6798
Naylor, A. R., Ricco, J.-B., de Borst, G. J., Debus, S., de Haro, J., Halliday, A., ... & ESVS Guideline Review Group. (2018). Editor's Choice—Management of atherosclerotic carotid and vertebral artery disease: 2017 clinical practice guidelines of the European Society for Vascular Surgery (ESVS).
European Journal of Vascular and Endovascular Surgery, 55(1), 3–81. Doi: 10.1016/j.ejvs.2017.06.021
Moore, K. J., Sheedy, F. J., & Fisher, E. A. (2013). Macrophages in atherosclerosis: A dynamic balance.
Nature Reviews Immunology, 13(10), 709–721. Doi: 10.1038/nri3520
Messas, E., Goudot, G. (2020). Management of carotid stenosis for primary and secondary prevention of stroke: state-of-the-art 2020: a critical review.
Eur Heart J Suppl. 22(Suppl M): M35–M42. Doi: 10.1093/eurheartj/suaa162
Dossabhoy, S., Arya, S. (2021). Epidemiology of atherosclerotic carotid artery disease.
Seminars in Vascular Surgery. 34 (1), 3-9. Doi: 10.1053/j.semvascsurg.2021.02.013
Jebari-Benslaiman, S., Galicia-García, U. (2022). Pathophysiology of Atherosclerosis.
Int J Mol Sci. 23(6): 3346. Doi: 10.3390/ijms23063346
Müller, М., Lyrer, P. (2020). Carotid artery stenting versus endarterectomy for treatment of carotid artery stenosis.
Cochrane Database Syst Rev. 2020 (2): CD000515. Doi: 10.1002/14651858.CD000515.pub5
Saba, L., Yuan, C. (2018). Carotid Artery Wall Imaging: Perspective and Guidelines from the ASNR Vessel Wall Imaging Study Group and Expert Consensus Recommendations of the American Society of Neuroradiology.
AJNR Am J Neuroradiol. 39(2): E9–E31. Doi: 10.1002/14651858.CD000515.pub5
Table of content
Thank you for your comment!
Your comment has been submitted for moderation and will be published soon. We'll email you once it’s live.